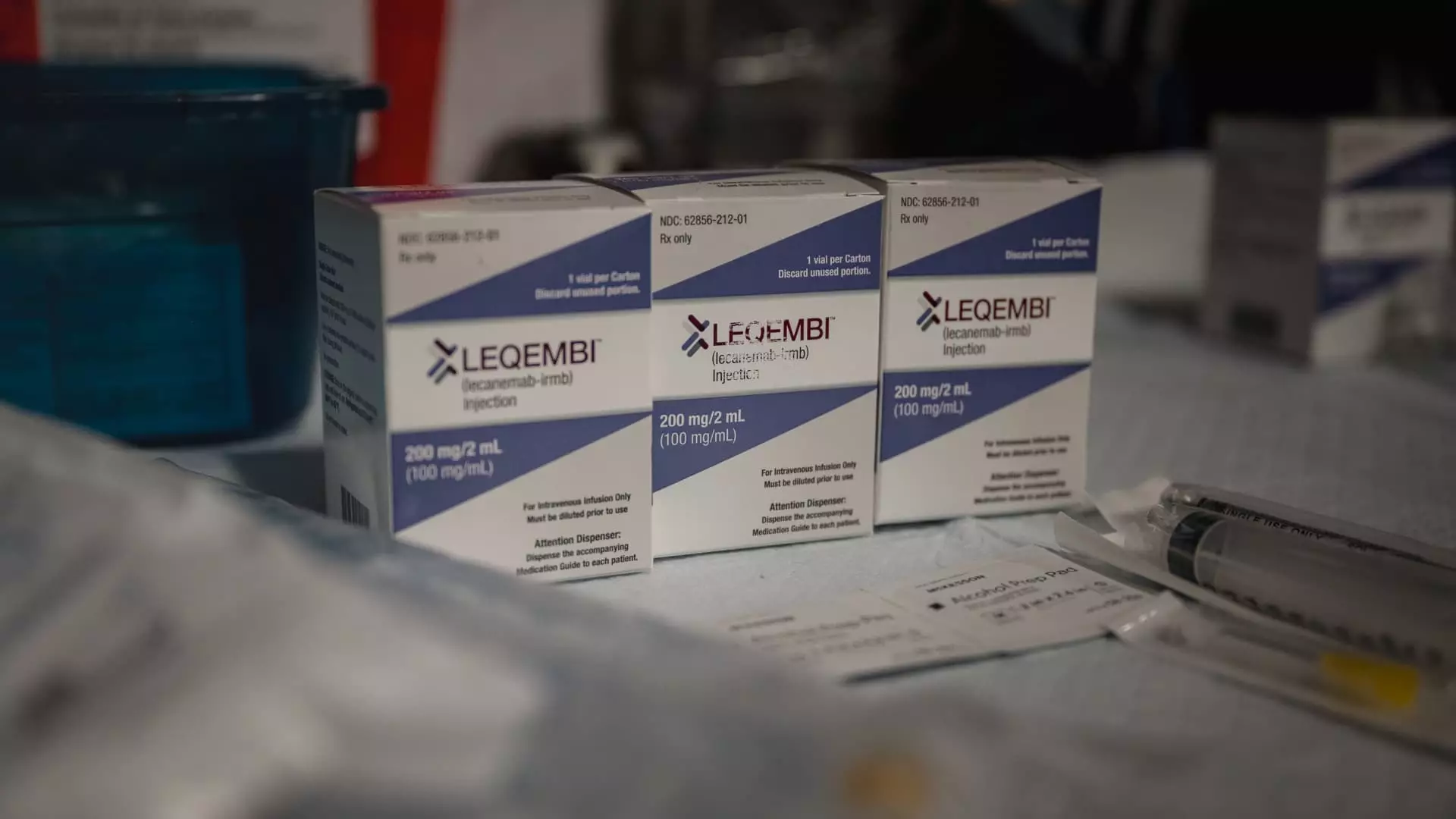
The latest data released by Japanese drugmaker Eisai showcases the positive impact of the breakthrough Alzheimer’s drug Leqembi on patients over an extended period of three years. The study results indicate the critical need for patients to remain on the treatment for an extended period to experience its long-term benefits.
One of the key findings from the study is the substantial drop in adverse side effects associated with Leqembi, such as brain bleeding and swelling, after six months of treatment. This decrease in adverse effects is crucial for ensuring the safety and efficacy of the drug. However, concerns raised by some doctors about these side effects led a European drug regulator to recommend against approving Leqembi last week.
The efficacy and safety data presented by Eisai highlight the significance of early and sustained treatment for individuals with Alzheimer’s disease. Leqembi, a monoclonal antibody that targets toxic plaques in the brain, demonstrates its ability to slow disease progression during the early stages. Despite not being a cure, the drug offers years of cognitive and functional benefits if administered early.
Future Treatment Possibilities
Eisai and Biogen are actively working towards expanding the treatment options for patients by seeking regulatory approval for a once-monthly infusion of Leqembi. Additionally, the development of an injectable form of the drug that can be self-administered at home on a weekly basis aims to enhance patient convenience and reduce the burden on the healthcare system.
The data from extended research on participants in mid-stage and late-stage trials reveal promising outcomes for patients receiving Leqembi treatment. Those who commenced the drug early experienced a slower rate of cognitive decline over three years compared to those who did not receive any treatment. This emphasizes the importance of early intervention in managing Alzheimer’s disease progression.
Furthermore, a sub-study focusing on patients with low levels of tau protein, a marker of Alzheimer’s severity, demonstrated notable results. Individuals with minimal or no tau levels experienced significant benefits from Leqembi treatment, with a majority observing no progression of the disease. This underscores the potential impact of the drug on patients at the early stages of Alzheimer’s.
The analysis of patients who temporarily discontinued Leqembi treatment revealed valuable insights into the drug’s long-term effects. While the positive impact of Leqembi was maintained even after treatment cessation, patients who stopped the drug experienced a reversion to the rate of cognitive decline seen in the placebo group. This suggests that sustained therapy with Leqembi is crucial for managing disease progression.
The latest data on Leqembi underscores the importance of continuous and early treatment for individuals with Alzheimer’s disease. The potential long-term benefits of the drug in slowing disease progression and preserving cognitive function highlight a significant advancement in Alzheimer’s research and treatment. With ongoing efforts to enhance treatment options and optimize patient outcomes, Leqembi offers hope for improving the lives of millions affected by this challenging condition.